Hip fracture
This is an anatomical impairment of the integrity of the femur, which practically does not respond to conservative treatment. In most cases, the pathology is treated by surgery, one of the types of which is osteosynthesis. Osteosynthesis in a hip fracture is an operation in which the reduction of fragments of the femur and their rigid fixation are performed.
Purpose of osteosynthesis
The main goal of the hip fracture operation is to recreate the correct position of bone fragments in the fracture zone, maintaining their immobility until the final fusion of the femoral neck.
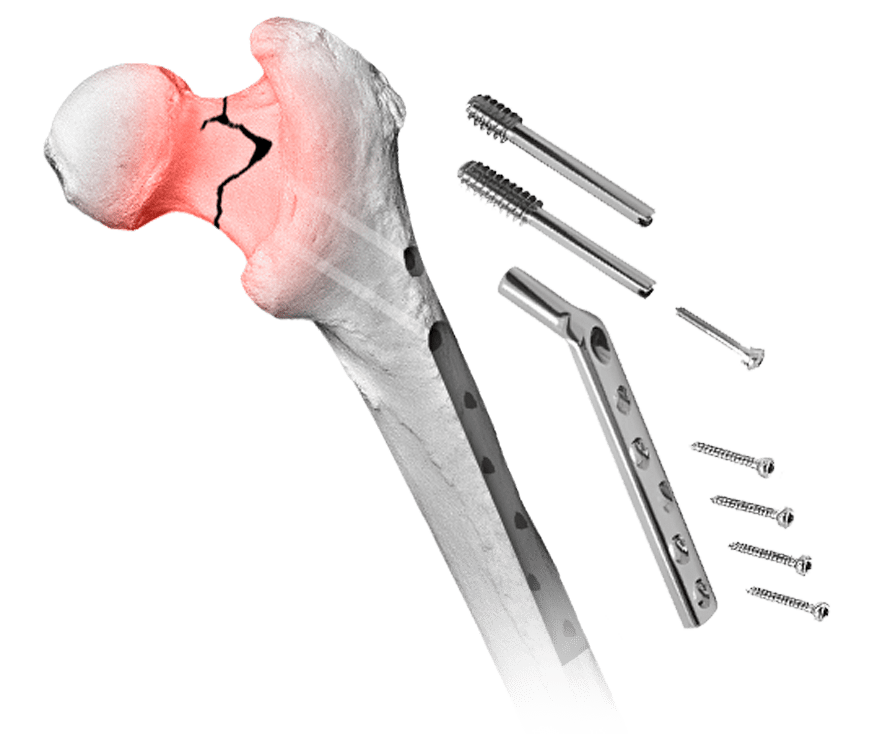
During hip surgery, various designs are used — metal spokes, threaded and rod systems (screws), devices with diaphyseal plates. Systems for osteosynthesis are made of special alloys of metal based on titanium or steel, which must be resistant to corrosion and biocompatible with the tissues of the human body.
Indications and contraindications for femoral osteosynthesis
Surgery of reposition (match in the correct position) of fragments in case of hip fracture is required in the following cases:
-
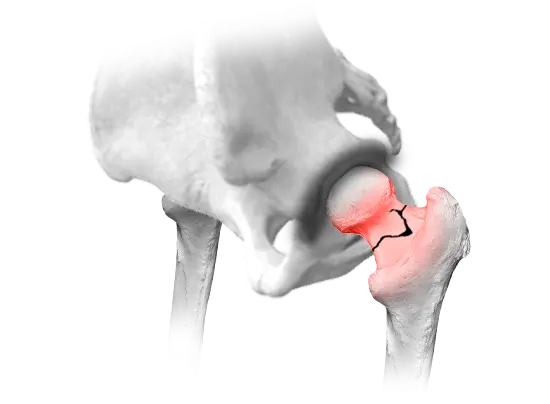
 Displaced fracture.
Displaced fracture.
-
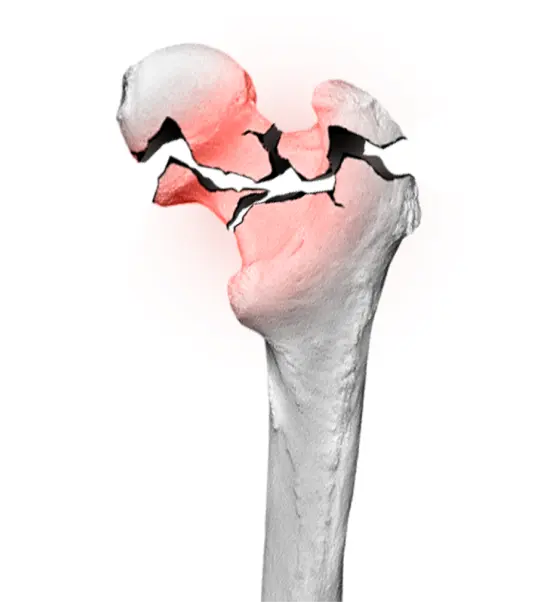
 Comminuted fracture.
Comminuted fracture.
-
 Combined injury.
Combined injury.
For example, a fracture combined with a dislocation. -
 Improper bone fusion, pseudoarthrosis, etc.
Improper bone fusion, pseudoarthrosis, etc.

- decompensated diseases of various organs and systems;
- severe general condition of the patient, shock, coma;
- infectious diseases, active form of tuberculosis;
coagulopathies; - purulent inflammations, skin, soft tissue, bone infection in the intervention area;
- severe mental impairment;
- severe lower extremity thrombophlebitis.
For a successful result of osteosynthesis in case of a hip fracture, its location, the degree of impaired blood supply to the bone in the injury area is also taken into account. Subcapital fracture with displacement, significant disruption of blood supply to the femoral head, the likelihood of aseptic necrosis significantly reduce the likelihood of successful intervention.
Отзывы пациентов
Methods of osteosynthesis
Osteosynthesis in hip fracture is performed by two main methods — extramedullary and intramedullary. Both of these methods are a type of internal (immersion) osteosynthesis, however, with the extramedullary method, the structural elements do not affect the medullary canal, and with the intramedullary one, they are passed through it.
Intramedullary method
Intramedullary osteosynthesis is one of the most effective treatments for fractures. It involves the introduction of special devices into the medullary canal of each of the bone fragments. These devices are rods, nails, which can be rigid or semi-elastic.
To ensure the stability of the system, there are screw holes or special bends on the distal ends of the fixing elements. Structures for intramedullary osteosynthesis can even fix fractures with many fragments.
The nails are inserted into the medullary canal after pre expansion or without it. After bone fusion, all intramedullary constructs are removed.
Extramedullary osteosynthesis
For osteosynthesis with screws in case of hip fracture, doctors use special plates, which are attached to the bone with fasteners.
Preparation for hip
osteosynthesis surgery
In case of a fracture of the femoral neck, surgery is recommended to be carried out as quickly as possible, so preparation for it should take place in an accelerated mode.
To confirm the diagnosis of hip fracture, and to determine its nature, radiography is carried out. Computer or magnetic resonance imaging will help to assess the degree of impaired blood supply to the fracture area, which affects the possibility of osteosynthesis.
Standard preparation includes cleansing the intestines with an enema or special drugs the night before and on the morning of the operation, removing hair in the surgical area. The last meal (light dinner) should be 8-10 hours before the intervention, it is done on an empty stomach, you cannot eat or drink on the morning of the operation.
It is necessary to obtain the medical conclusion of the attending physician about the possibility of surgery.
On the previous night or immediately before the operation, the patient talks with an anesthesiologist, who will find out whether surgical treatment was carried out earlier, what type of anesthesia was used, whether the patient is allergic to drugs, whether he abuses alcohol, what medicines he is on.
This data will help the doctor choose the optimal anesthetic support. In most cases, osteosynthesis for femoral neck fracture is performed under general anesthesia. In some cases, epidural anesthesia is possible.
The patient is also prescribed an additional examination:
- complete blood count and urine tests;
- biochemical blood test, determination of blood type and Rh factor;
- hemostasiogram;
- a test to determine indicators of mineral metabolism (phosphorus, calcium);
- densitometry;
- ECG;
- Photofluorography or chest X-ray.
- Detailed (clinical) complete blood count with platelet count, up to 14 days.
- Urinalysis, not more than 14 days.
- Biochemical blood test (ALT, AST, total and direct, bilirubin, blood glucose, total protein, urea, creatinine, sodium, calcium, potassium, chlorine), for no more than 14 days.
- Coagulogram (fibrinogen, APTT, prothrombin time, Quinque prothrombin time, INR, thrombin time, clotting time and bleeding duration), up to 14 days.
- Blood test on hepatitis markers In (HbsAg) and hepatitis C (HCV), no more than 3 months.
- Blood test on RW, up to 1 month.
- Blood test on HIV infection, no more than 3 months.
- Blood type, Rhesus factor, up to 2 months.
- Phenotyping of erythrocytes on Rh system antigens (C, E, c, e) and Kell antigen, it is termless
- Alloimmunny anti-erythrocyte antibodies, including antibodies to Rh-antigen
- The electrocardiogram (ECG) with interpretation and the conclusion, up to 14 days.
- Fluorographic examination of the chest organs or a chest X-ray in 2 projections, for a period not exceeding 6 months.
- Fibrogastroduodenoscopy, not more than 3 months. In the presence of ulcerative history, erosion of the gastrointestinal tract, not more than 1 month.
- Ultrasound examination of the veins of the lower extremities, up to 1 month.
- Ultrasound examination of the arteries of the lower extremities, for a period not exceeding 1 month.
- Ultrasound examination of brachiocephalic arteries, not more than 3 months.
- Echocardiography (cardiac ultrasound), not more than 1 month.
- Daily ECG monitoring, for individuals with hypertension over 65 years of age, not more than 1 month.
- TSH, glycated hemoglobin, for individuals with diabetes mellitus, not more than 14 days.
- Conclusion from the therapist in printed form, indicating the absence of contraindications to surgical treatment and indicated concomitant diseases, up to 1 month
- Conclusion from narrow specialists (oncologist, endocrinologist, cardiologist, etc.) complete examination, in the presence of concomitant diseases, not more than 1 month
- X-ray of pelvic bones with capture of the upper third of the thigh, femur in one projection on the film at 100% scale. (In one image, both joints are in direct projection).
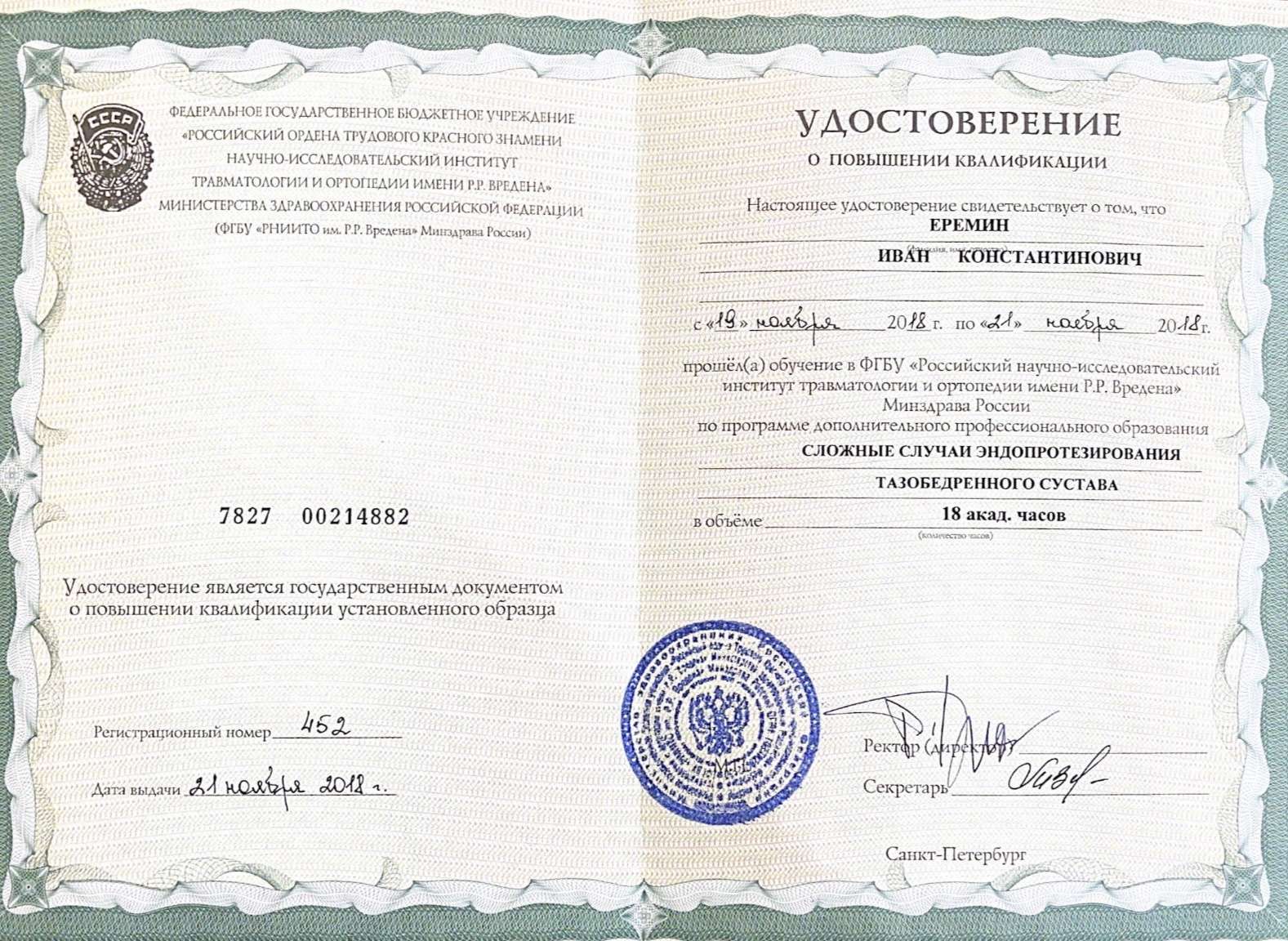
Center staff
Operation progress
The patient is placed on the operating table and put into anesthesia. During the operation, they will not feel anything and will come to their senses in the intensive care unit, where they will be under close supervision of medical personnel.
The limb is fixed in the desired position. The operating field is treated with an antiseptic. Then the surgeon makes an incision, the size of which is from 2-3 to 10-15 cm, depending on whether a closed or open reposition is carried out.
In closed intramedullary osteosynthesis, the fixation construct is inserted at a specific point in the femoral head under radiographic control through a 2-3 cm incision by screwing in and using special instruments.
Open osteosynthesis involves an extensive incision (up to 10-15 cm), comparison of bone fragments, installation of the selected fixation system.
The final stage of the operation is the treatment of the wound, its drainage, and suturing. If the chosen technique involves immobilization of the limb, a plaster cast is applied to the patient.
Possible complications
Osteosynthesis of the femoral neck can be accompanied by general complications inherent in any surgical intervention, and specific. Common complications include infections, fat or air embolism, congestive pneumonia, deep vein thrombosis of the limb.
To avoid complications, the surgeon must carefully assess the possibility and feasibility of osteosynthesis before surgery, and follow all aseptic and antiseptic rules during the intervention. The patient should strictly follow all the recommendations of the doctor in the postoperative period.
Specific complications of osteosynthesis:
- aseptic necrosis of the femoral head;
- non-union of bone fragments;
- impaired stability of fixation, disconnection of bone fragments;
- osteomyelitis of the femur;
- false joint formation;
- arthrosis, hip arthritis.

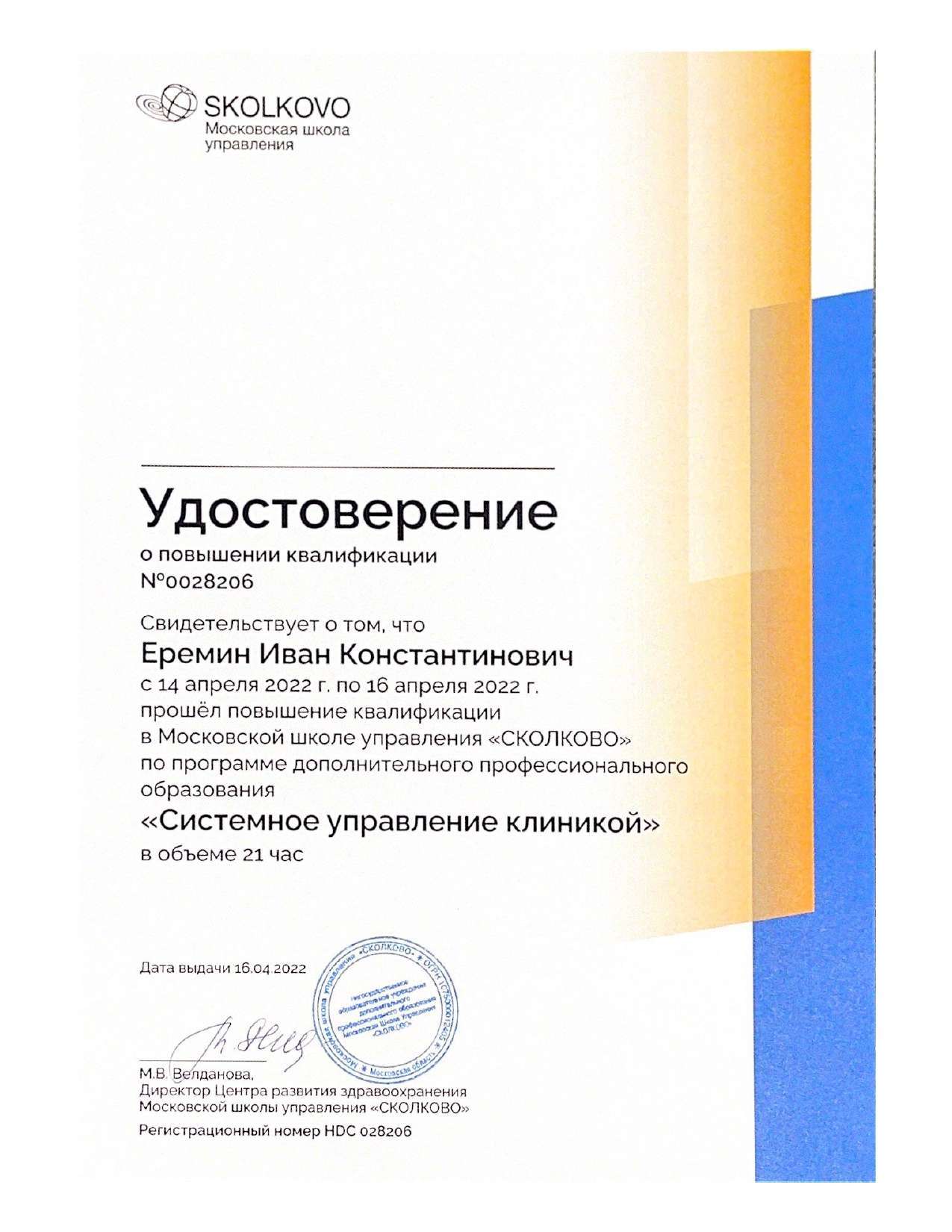
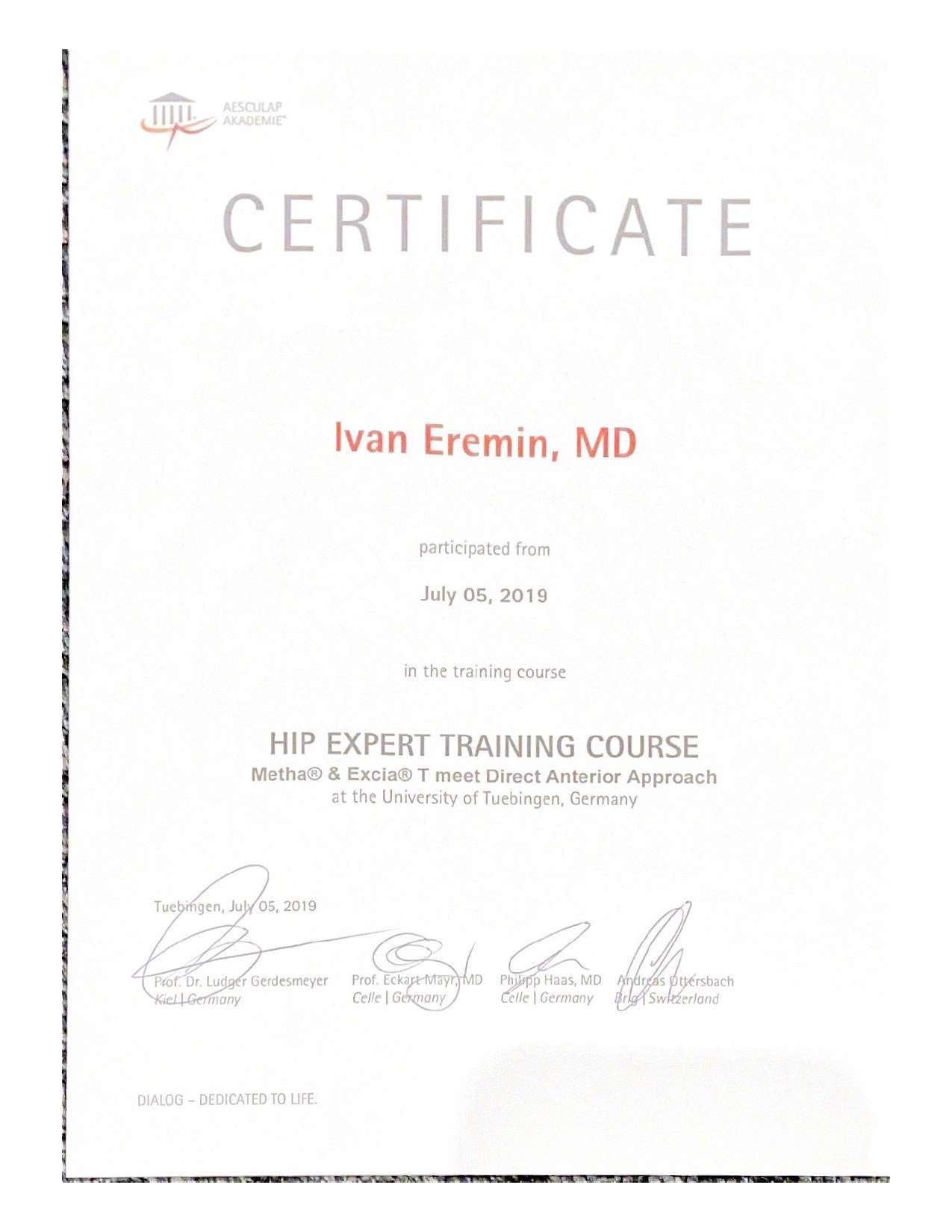
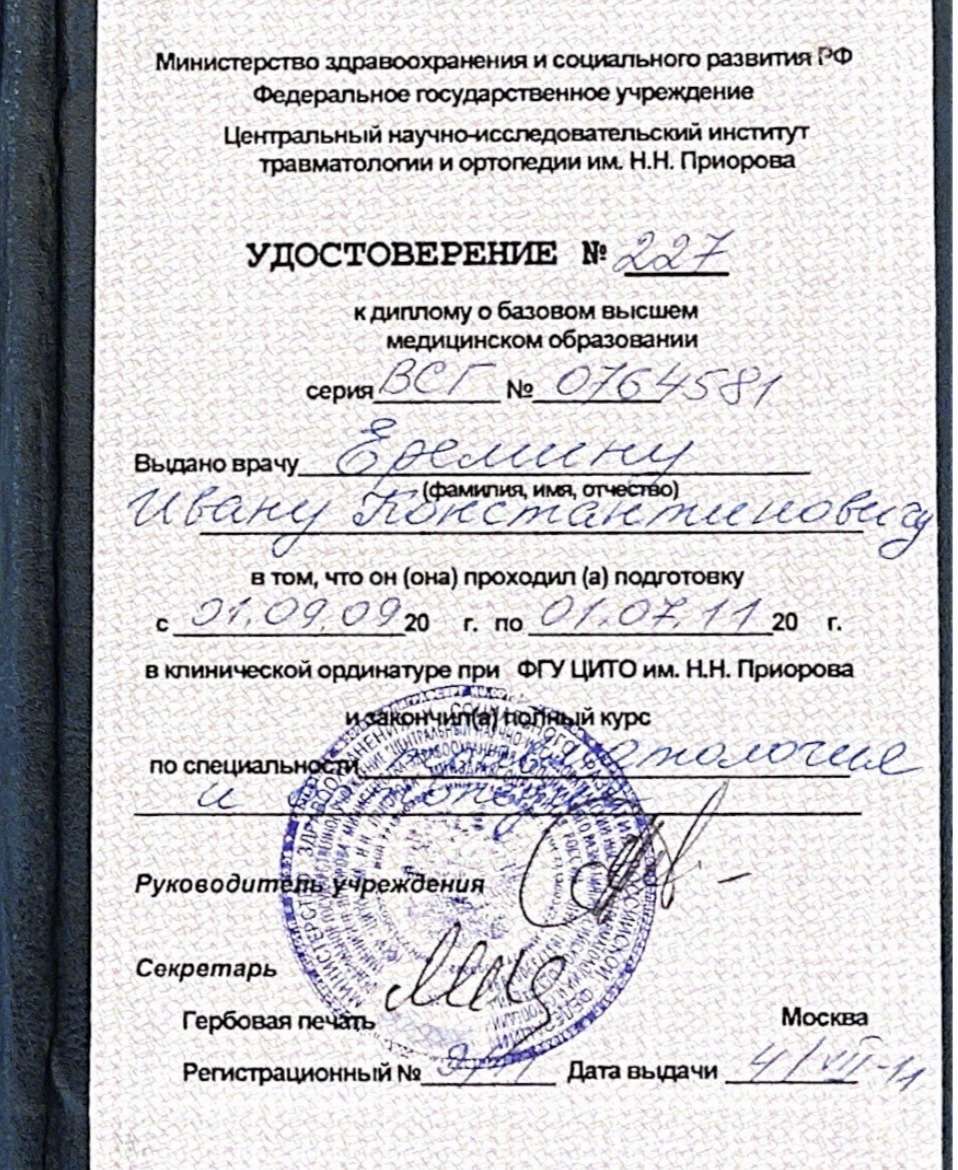
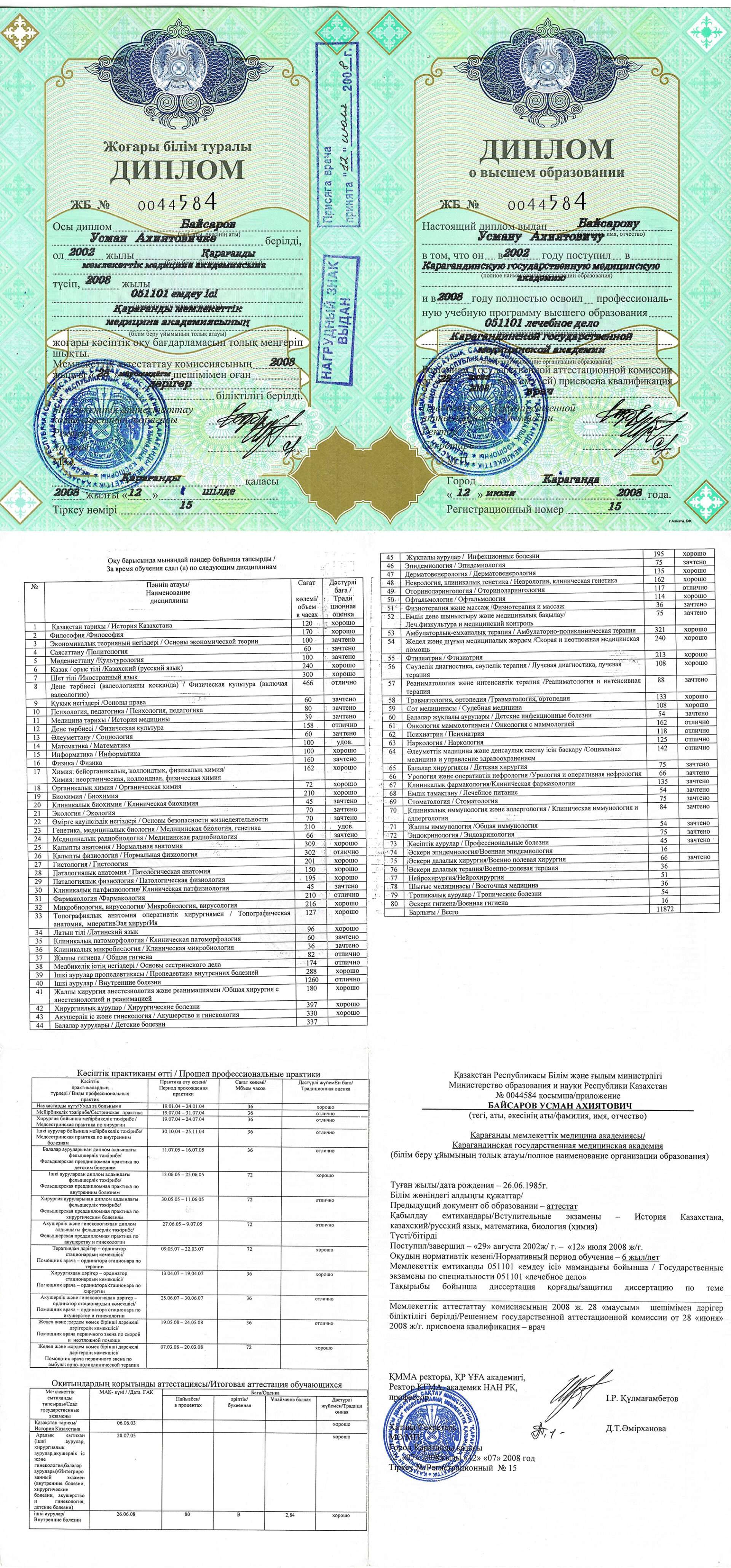
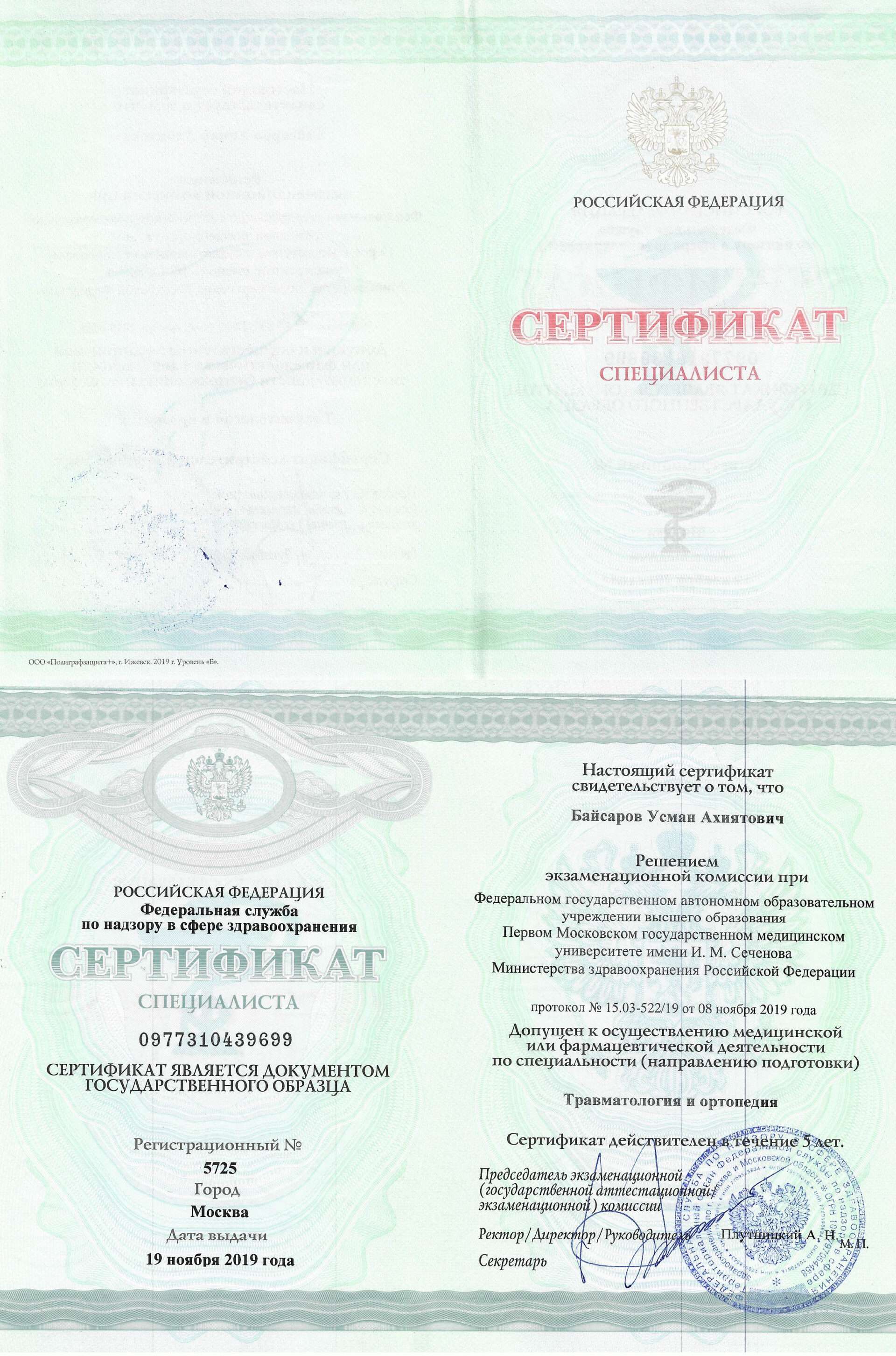
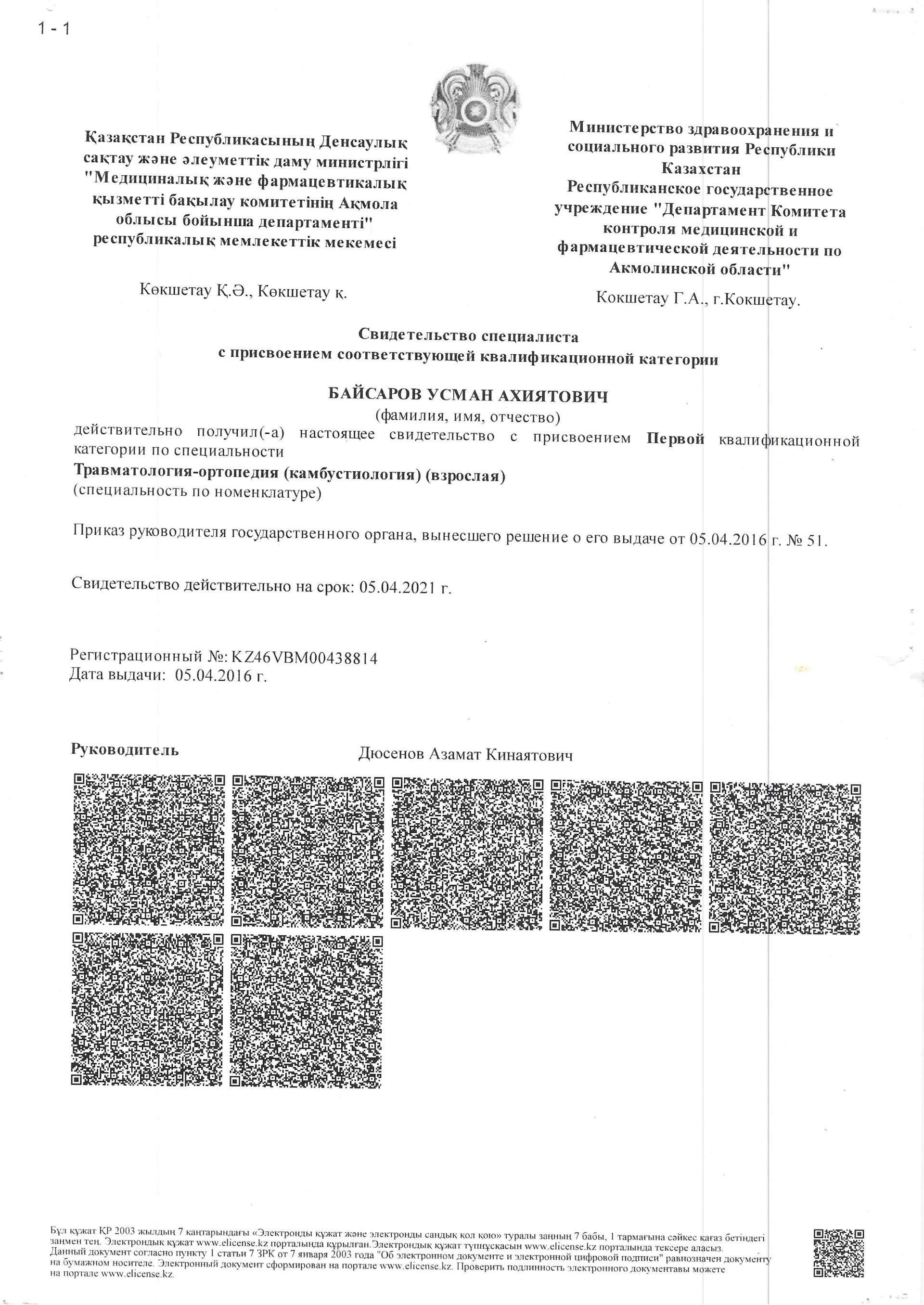
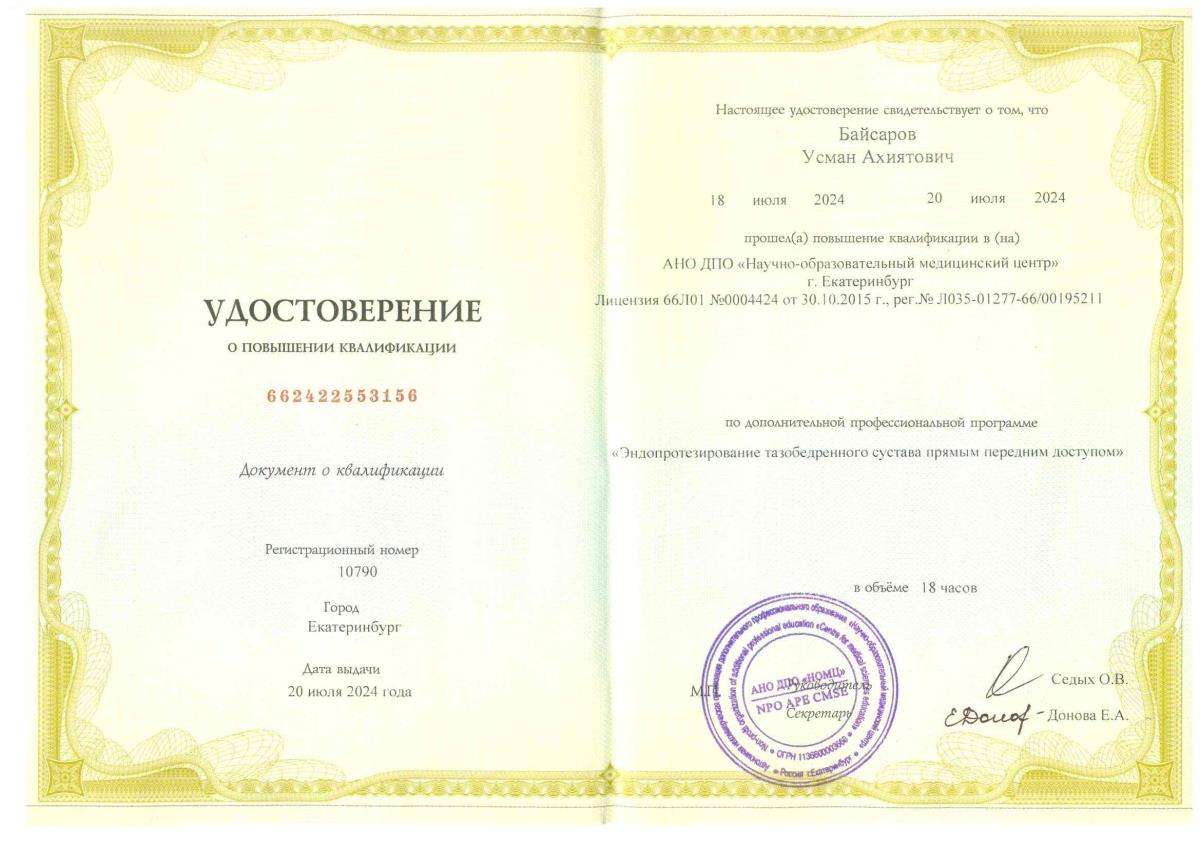
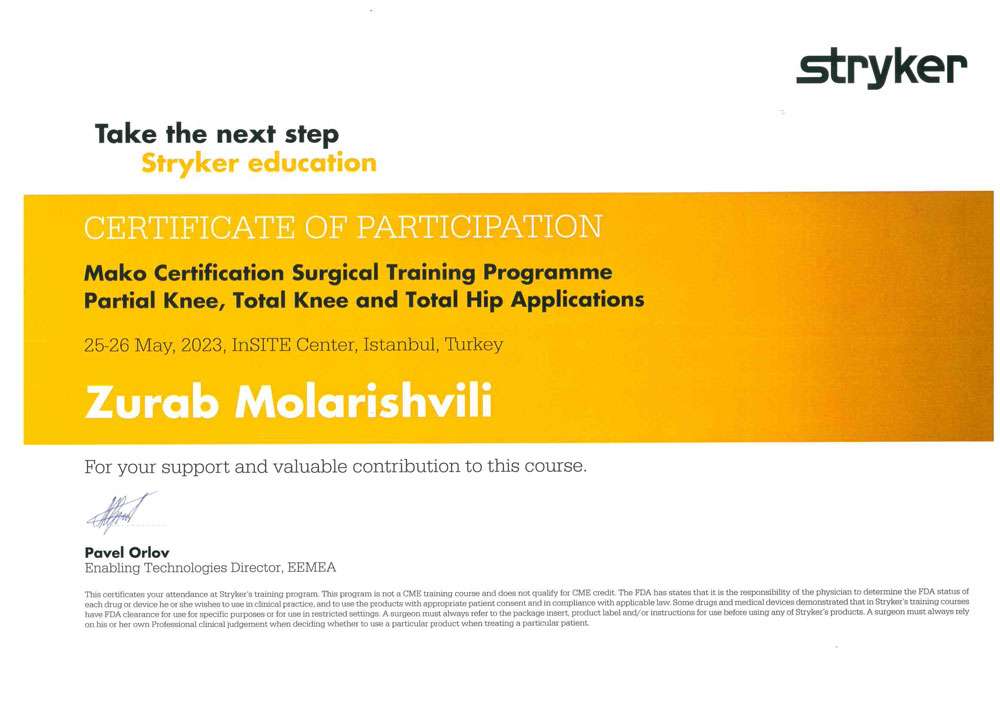
At the Hip Surgery Center, osteosynthesis for hip fracture is carried out using modern methods and high-tech equipment. Experienced doctors of the clinic are constantly improving their qualifications, using only the best experience in their activities.
Employees of the Center make every effort to ensure that the treatment process, recovery of patients proceed as quickly as possible, comfortably and with the best results.
Rehabilitation
Immediately after the operation, the patient is transferred to the intensive care unit or ward, a cold compress is applied to the place of intervention, antibiotic therapy, painkillers, and, if necessary, other drugs are prescribed. Bed rest after surgery should not be long, maximum 1-2 days, early activation contributes to the prevention of postoperative complications, faster recovery. However, the load on the operated limb should be reduced, the patient should move using crutches. In the early recovery period, breathing exercises and massage are carried out to prevent congestion. It is necessary to treat the sutures, which are removed in 10-12 days.
After the operation wound is healed, the patient is prescribed recovery procedures, the number and intensity of which increases gradually. These include:
- physiotherapy exercises — passive and active exercises, exercises on simulators;
- physical therapy;
- therapeutic baths;
- paraffin wraps;
- massage;
- swimming, aquagymnastics.
The time to fully restore the functions of the limb and return to the usual way of life depends on many factors: the patient’s age, state of health and physical shape in general, the severity of the fracture, the absence or presence of postoperative complications. The rehabilitation period can take from 3-6 to 12 months.

Don’t let joint pain define your life
Give yourself freedom of movement without restrictions
Over 5 years, using the DAA method, we returned more than 3 thousand patients to an active life.